PHOENIX — An Arizona Army veteran who spent years in military service, emergency medicine and law enforcement is now part of a pioneering effort led by one of the country’s most prominent psychedelic researchers.
Nick Jones, a former member of the 82nd Airborne Division, is participating in a first-of-its-kind FDA-approved clinical trial overseen by Dr. Sue Sisley at the Scottsdale Research Institute, which will test whole psilocybin mushrooms in group therapy settings for police, fire personnel and military veterans.
Jones, who joined the military at 18 and later worked as a paramedic and police officer, said repeated exposure to trauma pushed him to rethink his future. After leaving law enforcement, he enrolled in Arizona State University’s graduate program for mental health counseling, hoping to help others who’ve experienced similar struggles.
“It’s about being able to help the helpers,” Jones said. “First responders and veterans go through things most people can’t imagine. Psychedelic therapy can help people process trauma at a fundamental level.”
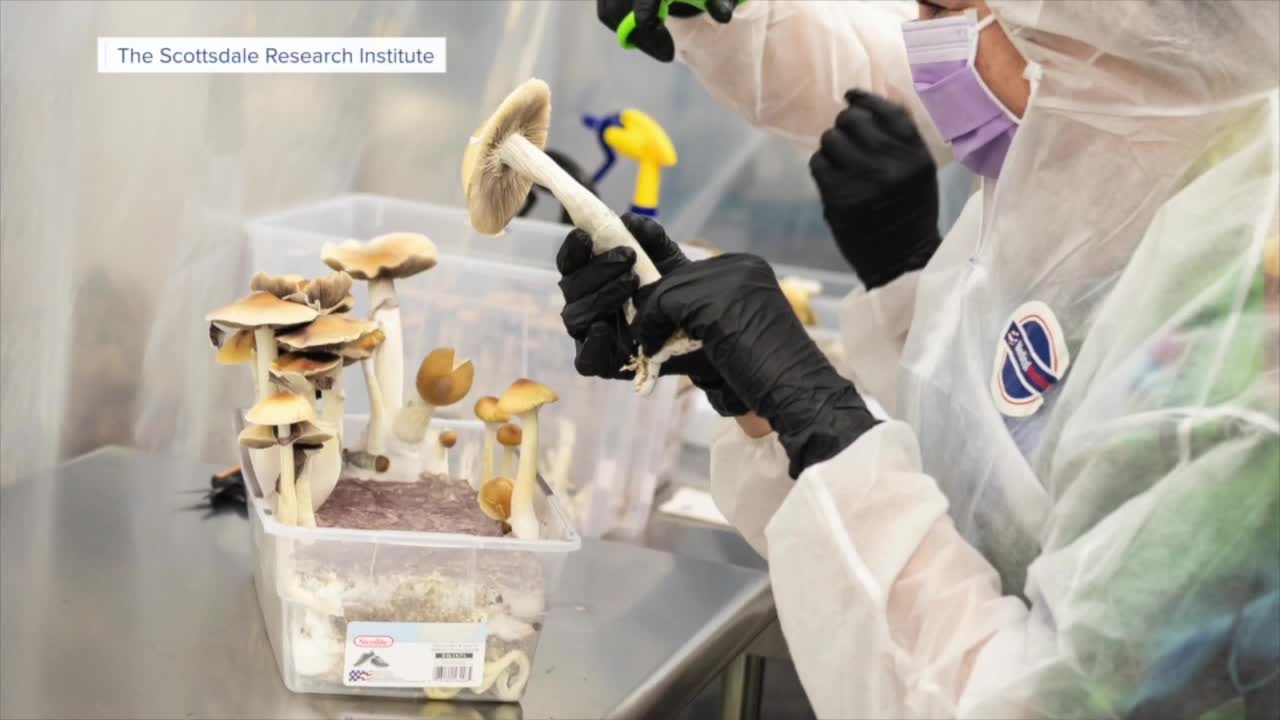
His experience is now intersecting with Dr. Sisley’s landmark study, believed to be the first controlled clinical trial in the world examining whole psilocybin mushrooms — not synthetic isolates — for trauma-related mental health conditions.
Researchers led by Dr. Sisley have launched the FDA-approved phase one study at her Arizona facility, where 24 participants will take part in supervised group sessions. Each will receive a standardized 30-milligram dose of whole psilocybin mushrooms in what she calls a carefully monitored “group dosing room.”
“I would say the experience is going to be probably more unique than anything else they’ve ever done, because they all consume the investigational drug here in this room,” Sisley said, pointing to a room with beds and soft lighting. “The psychedelic medicine gets absorbed, and it allows you to access certain parts of your brain that may have been dormant for years.”
The trial will evaluate safety, efficacy and whether group-based psychedelic experiences can support healing for PTSD and other trauma-related conditions.
In a groundbreaking approval, the FDA authorized the use of therapy dogs during dosing sessions to provide comfort when participants enter altered states — an innovation intended to maintain boundaries and avoid the risks associated with human touch.
“The FDA approved our study to utilize psychedelic therapy dogs to support patients who are in altered states of consciousness,” Sisley said. “The dogs are very intuitive. They know what people need.”
Psilocybin remains illegal in Arizona, something Sisley emphasized.
“Currently in Arizona, they do not have any allowance for people who want to do mushrooms legally,” she said. “There’s no decriminalized market. So, this FDA clinical trial is the only legal avenue for first responders and veterans.”
Interest in the study has surged far beyond capacity.
“This phase one trial only enrolls 24 subjects,” Sisley said. “The list of firefighters is almost at 300 now, and the police officers are over 50.”
Dr. Sisley said researchers are screening candidates daily. “We have police, fire, military veterans at the lab every day screening with our medical staff to figure out if they’re healthy enough to be in the trial and if they meet the inclusion and exclusion criteria.”
Ultimately, only eight participants from each group — police, fire and veterans — will be selected for the first phase.
Once participants take the mushrooms, the experience follows a structured therapeutic arc.
“They lay down, they start absorbing the music playlist,” Sisley said. “After that, they begin their integration process. We start doing sessions with them as a group where they are able to process what they experienced together.”
Researchers will gather data using independent raters, validated clinical tools for PTSD, depression and anxiety, and wearable devices such as Oura rings to track sleep and activity levels.
“We collect data on their sleep quality and activity level,” Sisley said. “All of our data gets put into the public domain — the good data, the bad data. Everything will be evaluated.”
Jones said his own microdose and moderate-dose psilocybin experiences — as well as ketamine infusions — showed him what psychedelic therapy could offer. “It’s profound,” he said. “It gives you a window to address things traditional therapies don’t always reach.”
Dr. Sisley hopes this phase one trial will lead to larger studies and eventually broader access.
“If the data looks compelling, and there is enough safety and efficacy, maybe there would be a way to expand,” she said.
For Jones, the work is personal — and urgent.
“We need to move fast,” he said. “So many people need help. Studies like this can make a real difference — not just for individuals, but for the communities they serve.”